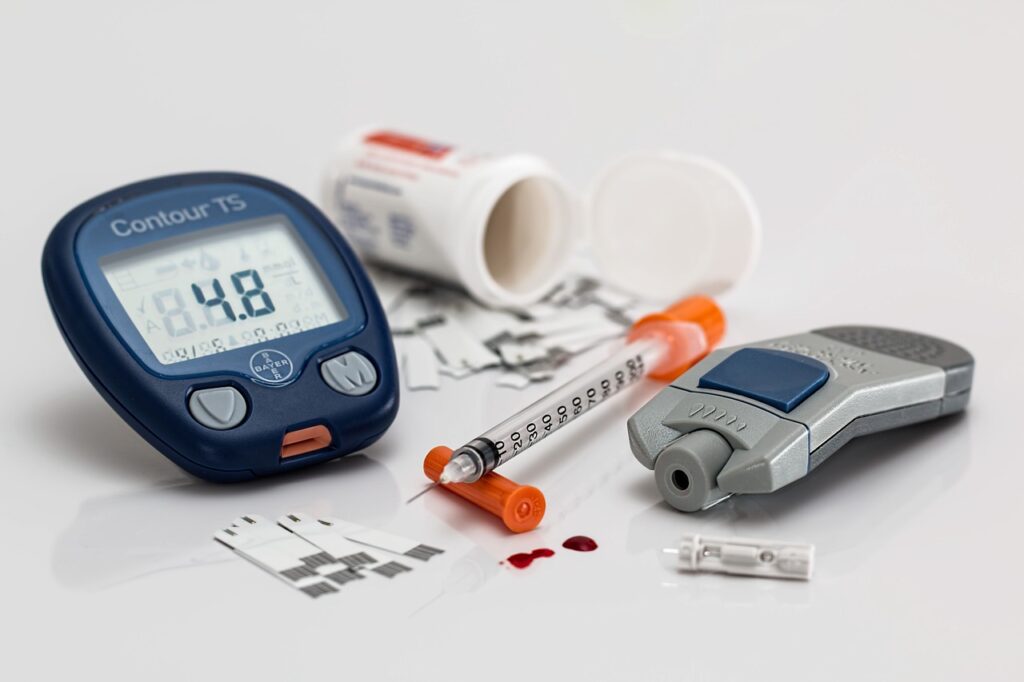
Washington [US], October 27 (ANI): Researchers have discovered a low-cost anti-inflammatory hydrogel that could one day be used to treat persistent skin lesions such as those observed in diabetics. In a paper published in the journal Biomedicine & Pharmacotherapy, they presented the results of animal studies.
According to the International Diabetes Federation, Brazil ranks sixth among countries with the most diabetes cases, which has reached epidemic proportions and has become the world’s fifth leading cause of death.
On a daily basis, 17.7 million Brazilians suffer from metabolic changes caused by decreased insulin secretion and action, including as nephropathy (kidney damage), neuropathy, and poor wound healing – one in every five diabetics is projected to develop chronic lesions such as foot ulcers.
In healthy persons, skin injury instantly initiates a chain of processes that leads to healing. Platelet aggregation regulates bleeding by providing binding sites for coagulation and cell growth. This is followed by the production of new blood cells and the deposition of collagen. High blood sugar levels (hyperglycemia) in diabetics, on the other hand, promote the creation of reactive oxygen species, which worsen inflammation and damage blood vessel development.
Biological hydrogels have successfully been used to accelerate wound healing, providing a moist and sterile environment. In this study, researchers at Sao Paulo State University (UNESP) and the Federal University of Sao Paulo (UNIFESP) developed a formula based on annexin A1 (AnxA1), a protein involved in regulating inflammation and cell proliferation, as evidenced by the group’s previous research.
The findings of this study showed that the hydrogel can modulate the wound microenvironment and favoured tissue regeneration. The effects of the hydrogel containing AnxA12-26 (a peptide synthesized using amino acids 2 through 26) were observed in mice with induced type 1 diabetes and skin lesions made with a biopsy punch.
The number of inflammatory cells was seen to decrease three days after the wounds were made. After 14 days, the wounds healed completely. In the control group, which comprised diabetic mice treated with a hydrogel that did not contain the peptide, acute wound inflammation continued beyond the third day.
Immunohistochemical analysis showed an improvement in tissue regeneration due to the proliferation of keratinocytes (cells that play a key role in restoring skin homeostasis and re-epithelization), reduced amounts of macrophages (immune cells that dampen inflammation, clear cell debris and coordinate tissue repair) and increased levels of vascular endothelial growth factor (VEGF), boosting the formation of new blood cells.
The cytotoxicity assay showed excellent biocompatibility and confirmed that the hydrogel is safe for use in treating diabetic wounds. “Our hydrogel is highly absorbent, providing the right amount of moisture to promote healing, which actually takes place faster than without it. It’s an effective option to expand the therapeutic arsenal for treating diabetic wounds,” said Sonia Maria Oliani, the last author of the article. Oliani is a professor at UNESP’s Institute of Biosciences, Letters and Exact Sciences (IBILCE) and UNIFESP’s Program of Graduate Studies in Functional and Structural Biology. (ANI)